Key Insights From Our Customer Webinar
In our latest webinar, MEG collaborated with St. John’s Hospital and its Senior Antimicrobial Pharmacist, Carol Johansson, to explore how the implementation of MEG’s Clinical Pharmacy Module revolutionised their pharmacy workflows. With challenges ranging from manual data entry to disjointed communication and risk management, St. John’s Hospital adopted a digital solution that streamlined processes, increased patient safety, and provided pharmacists with real-time data at their fingertips.
From Manual Processes to Digital Efficiency: A Pharmacy Transformation
Before adopting MEG’s Clinical Pharmacy Module, St. John’s Hospital pharmacists relied on cumbersome manual processes like Excel spreadsheets to track patient data, conduct medicine reconciliation, and document interventions. This approach was time-consuming, increased risk, and lacked the necessary data persistence, making it difficult to retrieve patient information during readmissions.
MEG’s Clinical Pharmacy Module automated many of these processes, allowing real-time tracking of patient data, prioritising high-risk patients, and facilitating multidisciplinary communication. The cloud-based system enabled the pharmacy team to focus on critical patient needs while ensuring compliance with safety protocols and regulatory requirements.
Main Dashboard Interface AND Patient Admissions (demo account)
Patients by Risk Rating (demo account)
Task Status (demo account)
Tasks by Handler (demo account)
Key Takeaways From St. John’s Hospital’s Success with MEG
Key Insight 1: Streamlined Workflow with Customisable Dashboards
MEG’s Clinical Pharmacy Module provided St. John’s Hospital with a dashboard that displayed essential patient information, such as bed numbers, risk scores, and medicines reconciliation status. Pharmacists could filter patients by risk, location, or ward, allowing them to prioritise tasks and manage workloads more efficiently. This helped reduce time spent on manual data management and improved decision-making processes.
Filtering by Risk Level (demo account)
Filtering by Location (demo account)
Key Insight 2: Streamlined Risk Scoring and Medicine Reconciliation
One of the major challenges for St. John’s was the manual risk scoring of patients, which was prone to inconsistency. MEG’s solution streamlined medicine reconciliation and task tracking, allowing pharmacists to efficiently prioritise high-risk patients and ensure they received prompt attention. The system also provided the ability to upload documentation and create standardised workflows for medicines reconciliation, which improved accuracy and safety.
Risk Scoring System Showing Patient Risk Categories (e.g. high, medium, low)
The medicines reconciliation status for each patient showing which patients have been reconciled or are pending (demo account)
The ability to upload documents related to patient care and medicine reconciliation tasks, showcasing how standardised workflows are integrated into the system.
Sample of the attached document (above)
Key Insight 3: Real-Time Task Management and Reporting
With MEG’s Clinical Pharmacy Module, St. John’s pharmacists could log, monitor, and complete tasks, from medicines reconciliation to risk assessments. The system’s tasks feature allowed pharmacists to assign tasks to specific team members, track the status of interventions, and ensure no patient was overlooked. This structured approach ensured clear communication across the pharmacy team and other healthcare professionals.
Tasks linked to a patient
Details of the task with handler, due date, status, and relevant intervention code.
Key Insight 4: Improved Multidisciplinary Communication
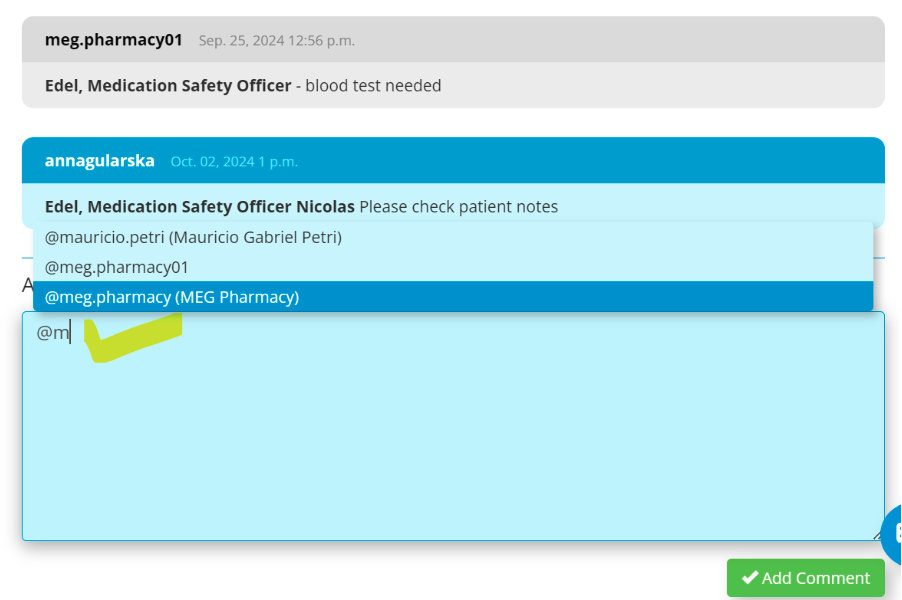
One of the module’s highlights was its ability to facilitate communication between the pharmacy team and other healthcare providers. Pharmacists could leave notes within patient records, alert colleagues to important updates, and tag team members to notify them of pending tasks. This streamlined handovers and ensured continuity of care, even when team members were absent.
Sample handover notes
Easily tag colleagues in notes and alert them to messages.
Boosting Patient Safety and Justifying Resources with Data-Driven Insights:
Since implementing MEG’s Clinical Pharmacy Module, St. John’s Hospital has seen a remarkable improvement in both efficiency and patient safety. In just two and a half years:
5,000 patients were screened through the system.
14,400 interventions were logged, including changes to medication, clinical reviews, and antimicrobial optimisations.
These interventions included over 5,500 related to medicines reconciliation, ensuring that patients were on the correct medications upon admission.
These results not only demonstrated the value of clinical pharmacy in improving patient care but also helped justify increasing staff resources, as the data showed a high volume of critical tasks that required pharmacist intervention.
Example of a KPI dashboard
Overview of task status
Action Planning overview dashboard
'Quick launch' of relevant forms and tools in other MEG modules (e.g. Medications Incident Report, Risk Register, MEG Patient Database) without leaving the Clinical Pharmacy module
Best Practices and Actionable Advice:
Prioritise High-Risk Patients with Custom Filters
The ability to filter patients by risk scores or location was crucial in ensuring that St. John’s pharmacists could focus their attention on those at the highest risk of medication errors. Carol Johansson emphasised the importance of configuring risk score settings within the module to reflect the hospital’s unique needs, ensuring the team remained focused on the most vulnerable patients.
Integrate Task Management into Daily Workflow
By automating tasks and assigning them to specific pharmacists, the team ensured accountability and transparency. This practice prevented tasks from being missed and allowed better prioritisation, as pharmacists were able to focus on urgent cases based on patient data.
Use Accessible Data to Support Resource Allocation
St. John’s Hospital was able to justify adding more pharmacists to their team by leveraging the easy access to comprehensive data provided by MEG’s Clinical Pharmacy Module. Before MEG it would have been very challenging to gather and organise the necessary data to highlight patient acuity and workload. With MEG, Carol Johansson and her team could easily access detailed information on interventions, task management, and patient needs, allowing her to compile accurate insights to support a strong business case for additional resources. The module provided clear visibility into the pharmacy team's activities and impact, enabling hospital management to make informed, data-driven decisions about resource allocation based on precise, accessible information.
Ensure Multidisciplinary Collaboration
Integrating the pharmacy module into the broader hospital workflow facilitated smoother communication between pharmacists, doctors, and other healthcare providers. Ensuring everyone had access to up-to-date patient information helped improve collaboration and patient outcomes.
Explore the Full Webinar to Transform Your Pharmacy Operations:
To learn more about how MEG’s Clinical Pharmacy Module can transform your hospital’s pharmacy operations, watch the full webinar recording here. For a deeper dive into the features, schedule a personalised demo with our team and discover how this solution can improve patient safety and streamline workflows in your healthcare organisation.